
I was so tired I could barely get my work done. I snapped at my family and shrunk my responsibilities to the bare minimum. I felt like I had a low-grade flu for years. Aches, pains, stabbing headaches, irritability, food intolerance, brain fog. Maybe mono? Menopause? When my oldest child started wrestling with similar symptoms, I started chasing information. It turned out, he had Lyme disease, babesiosis and other tick-borne infections. So did my other child. And so did I. I have no memory of a tick bite, nor do my children. It’s possible that I passed it to them in utero.

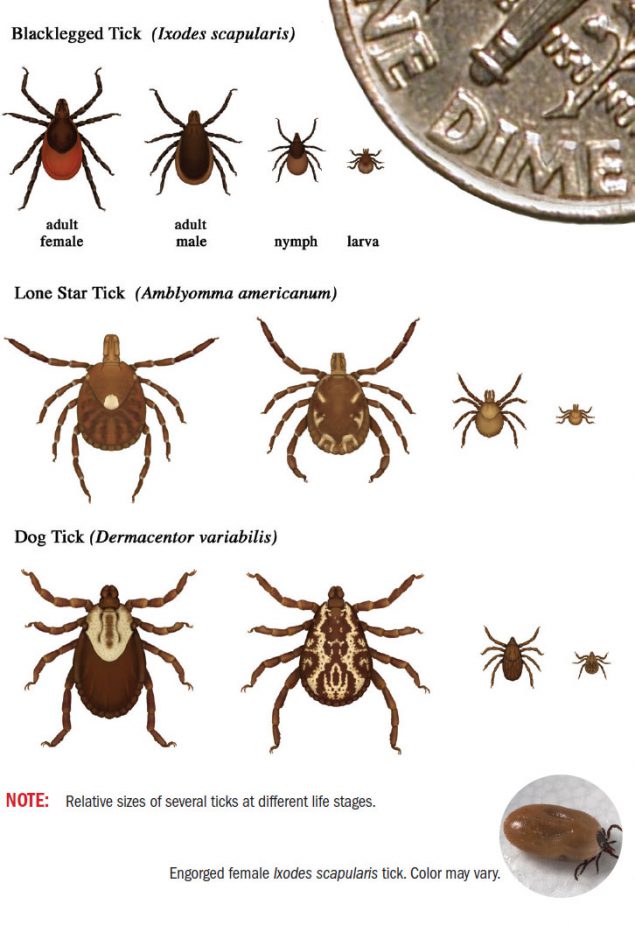
Ticks are tiny little critters, sometimes no bigger than the period at the end of a sentence. But the diseases they spread are big and nasty. And, we had several of them.
Lyme disease is the most well know of the tick-borne illnesses. Most of us know about joint pain and a bullseye rash, but the list of symptoms linked to Lyme includes fatigue, debilitating headaches, vision problems, nerve pain, brain fog, swollen joints, depression, and anxiety. There is a long history of controversy surrounding the prevalence, diagnosis, and treatment of Lyme. But even amid controversy, the Center for Disease Control (CDC) recently expanded its estimates of the prevalence of Lyme ten-fold. They now estimate there are nearly half a million new cases a year and they acknowledge many variations of a Lyme rash.
A lesser-known tick borne disease is babesiosis, a malaria-like red blood cell infection, is also becoming more prevalent. A fatal case recently made the Washington Post. Babesiosis causes flu like symptoms, fatigue, night sweats, anxiety, weight loss, sore feet in the mornings, and liver failure.
My family experience with tick borne infections includes multiple missed school years, missed work, extensive out of pocket medical treatment, lost social opportunities, isolation, and years of misdiagnosis by mainstream medicine. We were among the “lucky ones” who had the resources to chase treatment and largely recover. I say largely because every 2-4 years I take another round of antibiotic injections. Our journey was similar to the one shared in a recent Atlantic Monthly story, it was brutal and had life changing impacts for each of us.
Not everyone who gets a tick bite gets sick, and not everyone who gets sick winds up as debilitated as we did. But, I wouldn’t wish this journey on my worst enemy. A little knowledge and prevention can go a long way. I am not trained in the medical field, but I’ve spent over a decade trying to understand Lyme and tick-borne diseases. Here is what I have come to understand.
Prevention is key

- Ticks are nearly everywhere, and tick-borne diseases are horribly under reported. In one community on the west coast Lyme is nearly endemic but they chose not to discuss it for fear of losing tourism dollars.
- Wear light colored clothing with long pants tucked into socks. Check your clothing often.
- Stay on the trail, preferably in the middle. Ticks sit on tall grasses and leaves, waiting for something warm to stroll by.
- Avoid the “edges” of meadows, like the photo above, where the tall grass meets the trees. Edges attract deer and deer attract ticks. Same for those inviting rock walls; do not sit on them.
- Spray your clothing with permethrin products, especially shoes, socks and pants.
- Check yourself and your hiking partners frequently during and after time outdoors. Hair lines, groin, arm pits, anywhere that creases.
- Don’t wander out into fields or off trails in high tick season. I still go out, but I stick with wide, well-worn paths.
If you find an imbedded tick
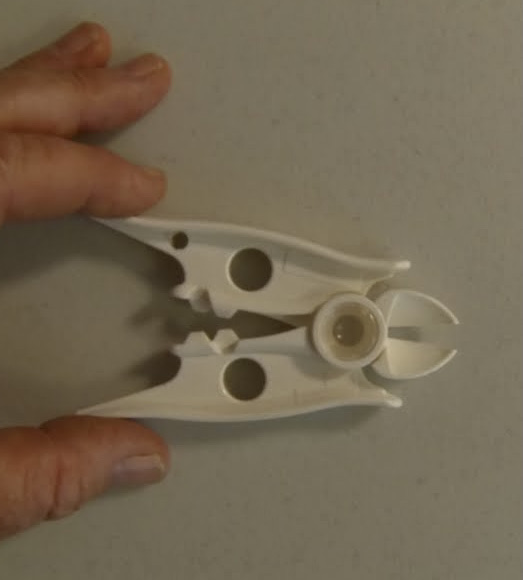
- No one really knows how long a tick has to be attached to start transmitting disease. If you find an imbedded tick, remove it with tweezers or tick nippers by pulling straight up.
- Immediately let your medical practitioner know. Many doctors, especially in endemic areas, will prescribe a 2 week course of doxycycline. Doxy is extremely effective at treating Lyme IF it’s caught early. If it were me, or my family, I would find someone to write a 6-week course of doxy. Many people believe it takes that long to treat an entire cycle of Lyme disease.
- Testing for Lyme and other tick borne illnesses is not very good yet and produces many false negatives. Just because you test negative doesn’t mean you don’t have a tick-borne illness.
- Consider saving the tick and send it to a lab to be tested for Lyme. This can run you $500 but, if it comes back positive you are in a better position to argue for longer treatment.
- If your symptoms continue beyond the 2-6 week doxy treatment window, or your practitioner won’t treat without a bullseye rash, consider looking for a Lyme Literate MD, LLMD. The International Lyme and Associated Diseases Society ILADS, lists doctors who treat Lyme with a variety of approaches.
Finally, if you are an avid outdoor person, with a gamut of odd symptoms, consider exploring tick-borne illness as a contributing source of your health issues. People with long undiagnosed Lyme seem to have multiple infections that can wreak havoc on the mind and body. It’s not always an easy or quick path to recover, but it is possible.
My experience with tick-borne illnesses has not dampened my love of the outdoors. But I take significant precautions. Bottom line, commit to a happy, healthy outdoor life and do your best to keep ticks at bay.
Mary Kirlin writes the column More Camper than Glamper, and spends as much time outdoors as she can.



